Table of Contents
The iron lung was a groundbreaking medical invention used to help patients breathe when their muscles couldn’t. Most commonly associated with polio treatment in the mid-20th century, the iron lung saved thousands of lives during respiratory paralysis. In this article, we’ll explain what an iron lung is, how it works, why it was so important in medical history, and where it stands in today’s world of advanced ventilators.
Nearly a century ago, one machine changed the future of respiratory care. But what exactly was the iron lung—and does anyone still rely on it today?
Back in the 1920s, a medical breakthrough helped thousands of people breathe when they no longer could on their own. Known technically as a negative pressure ventilator, this large cylindrical device earned a much more iconic name over time: the iron lung.
In this article, we’ll explore the purpose of the iron lung, how it worked, its role during the polio epidemic, and whether it’s still used in modern medicine.
A Giant Machine That Breathed for You
Imagine being completely conscious—but unable to take a single breath on your own. This was the terrifying reality for many polio patients in the early 1900s. For those who lost control of their chest muscles due to poliomyelitis, the iron lung offered something incredible: a second chance at life.
Though it looks like something out of a science fiction film—a giant metal tube with a human head sticking out—the iron lung was once a life-saving standard in hospitals. But how did this mechanical chamber actually work? And is it still used today?
In this article, we’ll cover:
- What an iron lung is
- How it helps people breathe
- Its historical impact during polio outbreaks
- Modern alternatives and whether it’s still in use
What Is an Iron Lung?
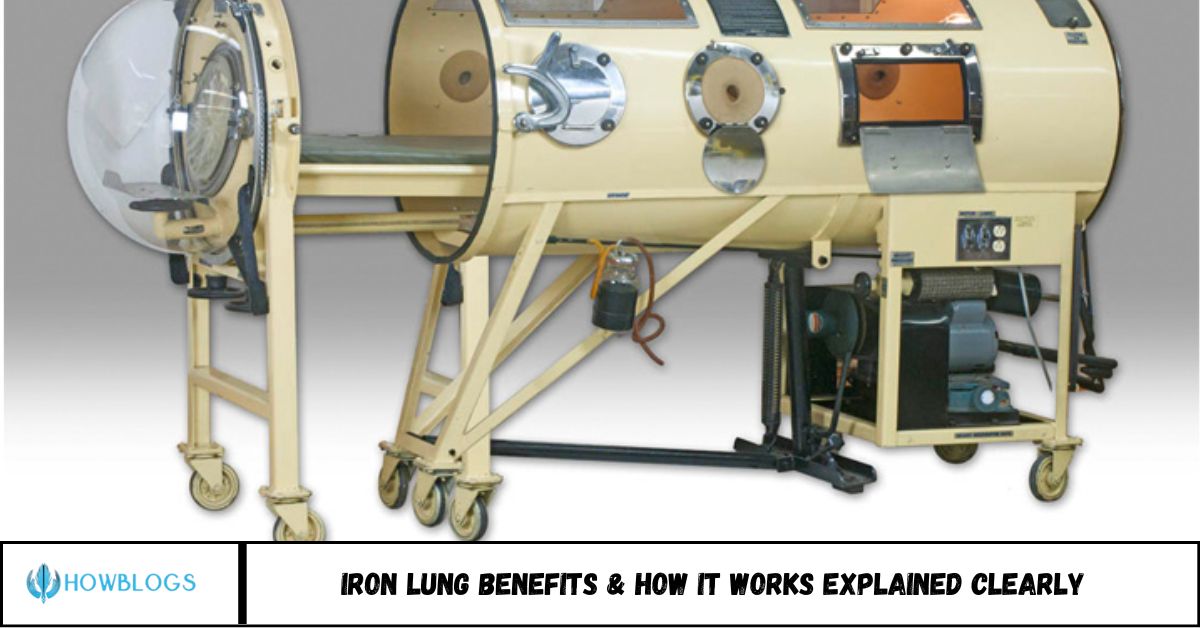
An iron lung, also known as a negative pressure ventilator, is a large cylindrical machine that encases the body (except the head) and mechanically assists with breathing.
It was primarily used to treat patients with respiratory muscle paralysis, especially those affected by polio in the early- to mid-1900s.
How Does an Iron Lung Work?
The iron lung uses negative pressure to mimic natural breathing:
Step-by-Step Process:
- The patient lies inside the chamber, sealed at the neck.
- A vacuum pump lowers the pressure inside the chamber.
- The reduced pressure causes the chest to expand, drawing air into the lungs.
- When pressure returns to normal, the chest contracts, pushing air out.
- This simulates the act of breathing—without needing the patient’s chest muscles to work.
Unlike modern positive pressure ventilators that push air into the lungs via a tube, the iron lung worked from the outside-in, using physics to help people breathe naturally
A Brief History of the Iron Lung
- 1928: First iron lung developed by Drinker and Shaw at Harvard.
- 1930s–1950s: Iron lungs were mass-produced due to polio outbreaks.
- 1952: During a polio epidemic in Copenhagen, over 2,000 patients required breathing support.
- 1960s and beyond: As vaccines reduced polio cases, iron lung use declined.
At its peak, thousands of Americans—many of them children—relied on iron lungs for daily survival.
Why Was the Iron Lung So Important?
Life-saving benefits included:
- Allowed patients to breathe without sedation or intubation
- Supported long-term survival for some (decades, in rare cases)
- Paved the way for modern ventilator design and respiratory medicine
Today, mechanical ventilators have replaced iron lungs in most settings. However, a few individuals still use them—often because their bodies have adapted or newer machines aren’t compatible.
Facts and Stats
- At the height of the 1952 polio epidemic, over 1,200 iron lungs were in use in the U.S.
- Vaccination programs (starting in 1955 with the Salk vaccine) nearly eradicated polio in developed countries by the 1980s.
- As of 2024, only one or two individuals in the U.S. are known to still rely on iron lungs.
Modern Alternatives to the Iron Lung
Today’s ventilators use positive pressure ventilation, which pushes air directly into the lungs via:
- Endotracheal tubes
- Non-invasive masks
- Tracheostomy tubes (for long-term use)
These are more portable, efficient, and adjustable, though they require skilled operation and may be more invasive.
FAQs
1. Is the iron lung still used today?
Rarely. Fewer than three people in the U.S. reportedly use them today, mostly due to personal adaptation and choice.
2. Why was the iron lung invented?
It was developed to help people breathe when polio paralyzed their chest muscles.
3. Does the iron lung hurt?
No. The process is non-invasive and not painful, though claustrophobia can be an issue for some.
4. How long did patients stay in an iron lung?
Some used it for weeks or months. A few, like Paul Alexander, lived in one for over 70 years.
5. How does it differ from modern ventilators?
Iron lungs use negative pressure; modern ventilators use positive pressure to deliver air into the lungs.
6. Who invented the iron lung?
Philip Drinker and Louis Agassiz Shaw built the first successful prototype in 1928.
Conclusion
Though largely a relic of the past, the iron lung remains one of the most iconic and important inventions in medical history. It saved countless lives during a terrifying era of infectious disease, gave birth to modern respiratory care, and still fascinates scientists and the public alike.
Today, the fight against diseases like polio continues—but thanks to vaccines and modern medicine, the iron lung has mostly retired, leaving behind a powerful legacy of innovation and hope.